The TIF® Procedure (Transoral Incisionless Fundoplication)
The TIF® procedure, or Transoral Incisionless Fundoplication, is an alternative to surgery for some patients with reflux symptoms.
The TIF procedure was introduced in 2005. The technique has undergone development and refinement over the years and has become an established treatment in some countries, especially the USA. Indeed, nearly 30,000 patients have now undergone the procedure.
Book a TIF® consultation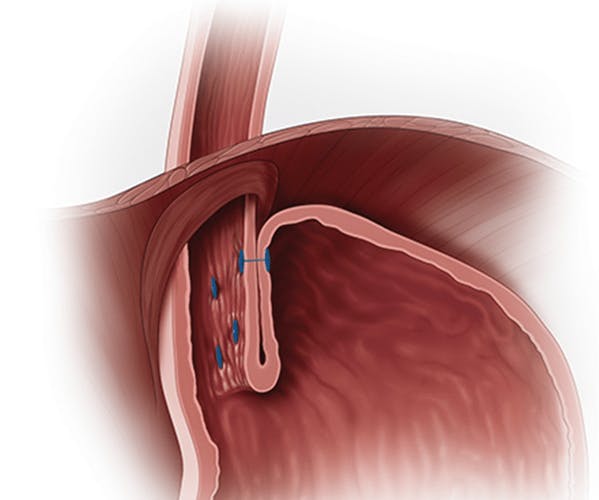
What is the TIF procedure?
Rather than strengthening the lower oesophageal valve in the standard way from inside the abdomen during a keyhole laparoscopic operation, during the TIF procedure it is approached from within the stomach using an “endoscopic” technique. Consequently, there are no cuts or scars on the abdomen. It is therefore less invasive than surgery.
Under general anaesthetic, the TIF instrument (EsophyX®) is placed through the mouth into the stomach. A standard gastroscope is inserted through a channel in the centre of the TIF instrument enabling the operator to inspect the stomach and to continually observe the procedure. Under direct visualisation, the instrument is then used to twist or “wrap” the top of the stomach, the fundus, around the bottom of the oesophagus and the two are then fused together using a series of plastic staples. In effect this employs the same principle as in standard fundoplication operations with the aim of strengthening the oesophageal “flap valve” with the intention of reducing gastro-oesophageal reflux. In essence a “partial fundoplication” is created.

These images show the EsophyX device inserted into the stomach (left), and the stapled ‘flap valve’ (right). Images provided, and use approved, by Endogastric Solutions®
Does TIF work?
In summary yes, but overall, probably not quite as well as surgery.
Many studies have been published to assess the safety and effectiveness of the TIF procedure. In 2021, a review of all the evidence at the time was published. According to this meta-analysis, TIF resulted in long-term patient satisfaction rates of 74% to 86%, with interruption/reduction of PPIs in about 75% of cases at 3 and 4 to 5 years, and with a significant and persistent improvement in GORD-related symptoms and quality of life in 80% and about 66% of patients at 4 to 5 and 10 years, respectively.
Does TIF work? Complications
These do occur after the TIF procedure as with any intervention, with early studies suggesting serious adverse events in up to 2% of patients. However, as the technique has been refined and experience has developed, the evidence is that complications are unusual. A review in 2019 of the industry gathered data from the MAUDE database in the USA of over 20,000 cases suggested that serious adverse events occurred in less than 0.5%. These can include;
- Oesophageal perforation
- Bleeding
- Injury to the stomach
- Infection
Side effects?
The side effects that occur after surgical fundoplication can also complicate endoscopic TIF, although they tend to be less troublesome and resolve quickly. These include:
- Sore throat
- Chest/abdominal/shoulder pain
- Difficulty swallowing (dysphagia)
- Difficulty belching/vomiting
- Abdominal bloating
Who should consider TIF?
The indications for the TIF procedure are broadly similar to those for any anti-reflux procedure. These include:
- Patients with symptoms poorly controlled by medications
- Patients who develop side effects on medications
- Patients who don't wish to take lifelong drugs, especially PPIs (Proton Pump Inhibitors)
- And specifically, patients who'd prefer to avoid traditional keyhole surgery
What if I have a Hiatus Hernia?
The exception is that many patients with reflux will have a hiatus hernia. If this is significant and not repaired, then it is less likely that patients will experience good symptom control. This is because as a hiatus hernia develops, the muscles of the hiatus are less able to exert pressure on the esophagus, and the bottom of the esophagus can move up into the chest. Consequently, this component of the lower esophageal sphincter fails.
During standard TIF procedures, it is technically impossible to repair a hiatus hernia. Therefore, in order to achieve a good outcome and restore normal anatomy, minimally invasive surgery is necessary. In standard Fundoplication, LINX® or RefluxStop™, if a hiatus hernia is present, it is always repaired to achieve good outcomes.
There is uncertainty as to what size of hiatus hernia excludes TIF procedures as an option. Most published studies include patients with hiatus hernias up to 2cm. However, even in early "small" hiatus hernias, there may be a significant hiatal defect (i.e., the hole in the diaphragm through which the esophagus passes, the hiatus is enlarged because of degeneration of its muscles), and failure to take this into account may compromise success in TIF.
Consequently, as with all patients undergoing any intervention, you'll need to undergo careful investigation and discuss the options with an expert clinician.
Concomitant Transoral Incisionless Fundoplication - cTIF™
This issue with hiatus hernias has led to the development of a combined procedure during which the hiatus hernia is repaired laparoscopically (involving a crural repair), and a fundoplication created endoscopically (TIF), theoretically combining the best of both worlds.
This procedure is becoming increasingly common in the USA and has been recently introduced to the UK by RefluxUK.

Pros & cons of the TIF procedure v surgery
Pros
- Least invasive of all anti-reflux procedures
- Compared to fundoplication, less invasive and thus theoretically lower risk of complications - however, remember that in expert hands, anti-reflux surgery is also low-risk
- No scars
- Rapid recovery
- Less side effects than standard fundoplication, including dysphagia and bloating
Cons
- Not suitable for patients with a significant hiatus hernia
- Probably less effective at controlling symptoms compared to laparoscopic surgery
- Long-term outcomes still relatively unclear
- LINX®️ avoids side effects of fundoplication, is now associated with low rates of dysphagia, and always includes repair of a hiatus hernia
Those interested in the evolution of the TIF procedure may wish to read this: Evolution of TIF
More Frequently Asked Questions About The TIF Procedure
Will I need a general anaesthetic?
Yes. The procedure requires a general anaesthetic.
How long is recovery?
You will return home on the same or following day as the procedure. You may experience a sore throat and pain in your chest and abdomen for 3-7 days.
Will I get side effects?
You may experience some swallowing difficulties (which usually resolve) as well as more bloating and wind if you can't belch as easily as normally, which affects 5-10% of patients.
Can I have another procedure if necessary?
Yes. The available evidence is that most patients achieve durable resolution of their symptoms, but if necessary, you can undergo 'redo' surgery.
Can I have the TIF procedure if I have a hiatus hernia?
If more than 2cm, no. If up to 2cm, it will depend on your clinician's assessment of the hiatal defect.
Are there any incisions?
No. It is incisionless.